
Healthcare DMS: How to Improve Patient Care With Document Management Systems

It’s 2 a.m. in the ER, and a patient arrives unconscious after a car accident.
The attending physician needs their medical history immediately, but the patient’s regular doctor’s office is closed, their paper charts are locked away, and their digital records are scattered across three different systems.
Healthcare professionals spend up to 35% of their time documenting patient information instead of actually caring for patients.
Meanwhile, HIPAA violations cost healthcare organizations an average of $9.77 million per breach, often because documents aren’t properly secured or tracked.
The reality is that healthcare facilities have figured out that Document Management Systems (DMS) solve both problems at once.
Think of a healthcare Document Management System (DMS) as your facility’s enhanced digital filing cabinet. It’s specialized software that organizes, secures, and manages all your medical documents in one place while keeping everything HIPAA-compliant.
What makes it different from basic document storage is that your healthcare DMS handles everything from patient charts and lab results to insurance claims and consent forms. Plus, it plays nicely with your existing Electronic Medical Records (EMR) and Electronic Health Records (EHR) systems instead of creating another headache.
The system serves as your backbone for medical records. It makes sure that critical patient information is always accessible to the right people while keeping detailed records of who accessed what and when.
Related: DMS vs. ECM
Healthcare organizations deal with document management challenges that would make other industries crumble. Here’s what your facility is probably dealing with right now:
| Challenge | Impact | DMS Solution |
|---|---|---|
| Patient Record Volume | Thousands of charts, lab reports, imaging results per facility | Centralized digital storage with instant search capabilities |
| HIPAA Compliance | $9.77M average cost per data breach (as of July, 2024) | Bank-level encryption and role-based access controls |
| Staff Productivity | 35% of time spent documenting patient information | OCR-powered search stores and retrieves any document in seconds |
| System Integration | Disconnected EMR, billing, and administrative systems | Seamless integration with existing healthcare software |
| Audit Requirements | Manual preparation for regulatory inspections | Automated audit trails and retention policy management |
| Interdepartmental Workflow | Paper-based handoffs between departments | Digital workflows from admissions to discharge |
Large hospitals deal with millions of documents across dozens of departments, while smaller clinics struggle just to keep basic records organized and secure.
Dental practices need lightning-fast access to treatment histories, and specialized clinics have to coordinate complex referral paperwork.
Without a systematic document management workflow, you’re looking at compliance violations, delayed patient care, and operational bottlenecks that hurt both patient outcomes and your bottom line.
Below is the general process you’ll follow while implementing a DMS in your healthcare facility.
Your first move is finding a vendor who actually understands healthcare compliance, like Dokmee.
You need a system that provides end-to-end encryption, detailed audit logging, and role-based access controls that’ll make HIPAA auditors smile.
Look for vendors who can show you their BAA (Business Associate Agreement) compliance and security certifications upfront. This foundation makes everything else possible, from training your team to integrating with your existing systems.
Healthcare staff are busy, stressed, and skeptical of new technology that might slow them down. Your approach matters.
Start with identifying individuals in each department who can become your internal advocates. These power users learn the system first and help their colleagues during the transition. Peer-to-peer support works way better than top-down mandates.
The real magic happens when your DMS integrates with your EMR/EHR, billing systems, and departmental workflows. You’re not creating another isolated system that everyone has to remember to check.
Good integration means patient documents automatically link to the right records without manual data entry. Your staff should be able to access the documents they need from within the applications they already use every day.
DMS implementation doesn’t end when you flip the switch.
Regular security audits and compliance reviews make sure your system keeps meeting evolving regulatory requirements as your facility grows.
Set up automated monitoring for things like
This proactive approach protects patient data while giving you the documentation needed for regulatory inspections.
When looking for a DMS solution for your healthcare facility, prioritize the following features:
Healthcare DMS security, more than passwords and firewalls, requires you to have multiple layers of protection that work together.
Modern healthcare generates documents in every format imaginable, from handwritten notes to complex imaging reports.
Your DMS needs OCR technology that can handle medical terminology and various document layouts and automatically extract key information like patient names, dates of service, and procedure codes.
This automated classification saves hours of manual filing while making sure documents end up in the right place and can be found when needed.
Your DMS should feel like a natural extension of your EMR/EHR system, not another platform you have to remember to check.
Documents should automatically attach to the correct patient records, and clinical staff should access what they need without leaving their primary applications.
This integration becomes especially valuable during patient encounters, where quick access to historical documents, lab results, and specialist reports can seriously impact care decisions.
Different medical documents have different retention requirements, and keeping track manually is a nightmare. Your DMS should automatically apply appropriate retention policies based on document type and regulatory requirements.
The system should also generate compliance reports for regulatory inspections, showing exactly:
This automated compliance documentation eliminates the weeks of manual preparation that typically happen before regulatory visits.
Integrating a DMS into your healthcare facility doesn’t only transform your workflows, it also brings over many advantages to your patients, too.
Remember that 2 a.m. emergency scenario?
With a properly implemented DMS, the attending physician can pull up that unconscious patient’s complete medical history, current medications, and known allergies in under 30 seconds.
That’s the difference between guessing and knowing.
This immediate access pays off in every patient interaction. No more delaying procedures while waiting for records from other departments, and no more making clinical decisions with incomplete information.
The interesting part is that the same patient information flows seamlessly between departments without anyone having to manually copy, fax, or hand-carry documents.
The emergency physician’s notes are instantly available to the ICU team, who can see the recent lab results and specialist consultations without making a single phone call.
For complex cases involving multiple specialists, everyone finally has access to the complete patient picture instead of working from fragments of information.
Modern patients expect to access their health information, and your DMS makes this possible through secure patient portals.
They can view lab results, discharge instructions, and care plans without calling your office, which reduces interruptions while improving satisfaction.
When patients can easily access and understand their information, they’re more likely to follow treatment plans and maintain better health outcomes.
All this organized documentation directly impacts your financial health.
Insurance claims process faster because billing staff can quickly access all supporting documentation without hunting through multiple systems.
Prior authorizations, referral paperwork, and treatment records get compiled and submitted efficiently. This reduces claim denials and speeds up payment cycles.
Many facilities find this improved cash flow pays for their DMS implementation within the first year.
Let’s look at some real-world uses of DMS in healthcare to concretize the importance of DMS in this field.
A regional medical center manages 50,000+ patient encounters annually across emergency, surgical, and outpatient services.
Before implementing their DMS, locating a complete patient file could take 15–20 minutes and often resulted in incomplete information during care decisions.
Their DMS solution creates unified digital patient folders that contain:
Now, when a patient arrives in the emergency department, staff can access their complete medical history within 30 seconds, including recent procedures, current medications, and known allergies.
This immediate access has reduced medical errors by a large percentage and improved patient satisfaction scores.
A clinic’s billing department was drowning in insurance paperwork, with claims processing taking 8–12 days and denial rates nearing 20% due to missing documentation.
Staff spent hours manually gathering supporting documents for each claim submission.
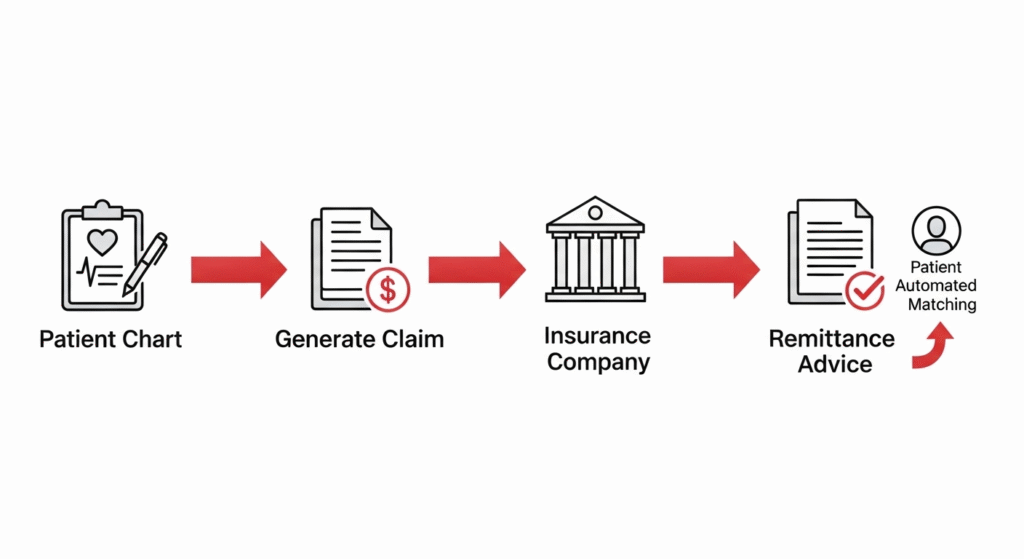
Their DMS implementation automated the claims workflow:
The result: claims processing time dropped to 3–4 days, denial rates fell below 10%, and the billing team could handle 40% more volume without additional staff.
A children’s healthcare network faced a comprehensive HIPAA audit that traditionally required months of preparation and inevitable disruption to operations.
Their previous audit preparation involved manually compiling documentation from multiple systems and departments.
With their DMS in place, audit preparation became routine:
The audit preparation that previously took 6 weeks was completed in 3 days, and the facility received 0 compliance violations.
The auditors commented on the thoroughness and organization of their documentation.
A university medical center’s research department manages 15+ clinical trials simultaneously, each generating thousands of documents, including consent forms, protocol amendments, adverse event reports, and regulatory submissions.
Their specialized DMS configuration handles:
This organized approach largely reduced startup time and eliminated documentation deficiencies during sponsor audits. The research team can now manage more studies simultaneously while maintaining the highest quality standards.
Ineffective document management doesn’t have to compromise patient care or compliance.
When every patient record, lab result, and administrative document is organized, secure, and instantly accessible, your entire facility operates more efficiently and safely.
Dokmee understands the challenges facing healthcare organizations and provides the specialized tools you need to eliminate document stress while ensuring bulletproof HIPAA compliance.
Our specialists can show you exactly how our healthcare DMS streamlines your workflows and protects your most sensitive patient data.
Schedule your free healthcare DMS consultation with Dokmee
A DMS enforces encryption, role-based access, and audit trails. Features like session timeouts, breach alerts, and login monitoring support HIPAA’s technical, administrative, and physical safeguards.
Yes. Leading DMS platforms like Dokmee integrate with Epic, Cerner, AllScripts, and others. Bidirectional sync enables clinical and administrative staff to access documents directly within EMR workflows.
Most facilities see ROI within 12–18 months through reduced document handling, faster billing cycles, and lower compliance risk. Long-term gains include storage savings and audit prep efficiency.
Immediate access to accurate patient data reduces errors and supports better treatment decisions. It eliminates illegible handwriting and maintains full documentation history.
Facilities typically digitize active files first, then archive records gradually. Hybrid workflows are supported during transition, and scanning services can accelerate the process.
Most organizations are fully operational in 3–6 months. A phased rollout by department minimizes disruption and allows staff to adapt smoothly